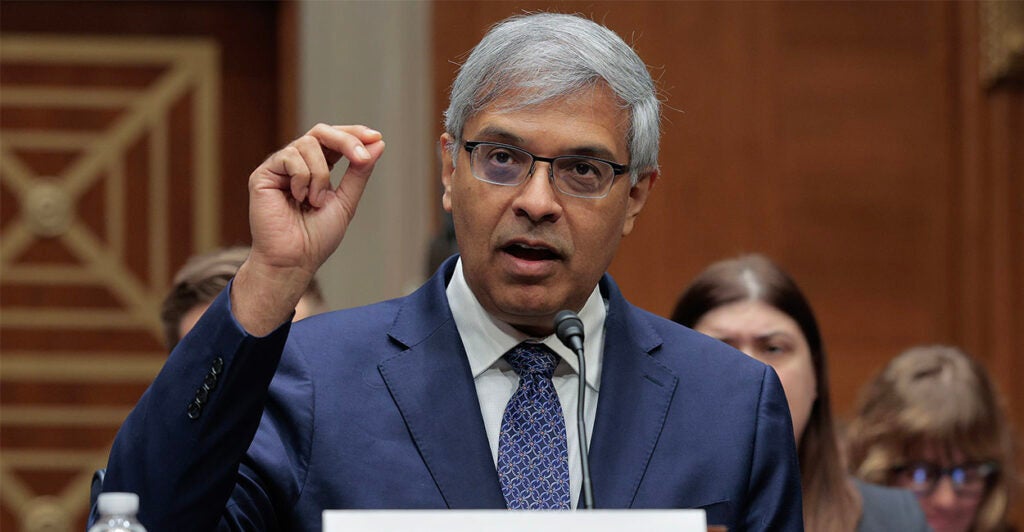
The news two weeks ago from the National Institutes of Health could be downplayed as a tidbit of politics by the Trump administration around the anniversary of the 1973 Supreme Court abortion decision. But that would be missing the larger import of the statement by NIH Director Jay Bhattacharya about the agency’s decision to end federal funding of research using tissue from elective abortions.
Bhattacharya said on Jan. 22, “NIH is pushing American biomedical science into the 21st century. This decision is about advancing science by investing in breakthrough technologies more capable of modeling human health and disease. Under President [Donald] Trump’s leadership, taxpayer-funded research must reflect the best science of today and the values of the American people.”
The announcement also stated that “NIH will continue to assess additional areas where modernization can accelerate progress and will engage the scientific community in identifying emerging technologies that can further reduce reliance on outdated research models.”
Is NIH seeking cover for an ideological decision that will set back scientific advances and the identification of cures for human maladies by decades or more? The record in this area provides strong evidence to the contrary.
Fetal tissue from elective abortion has been touted for years by some researchers as the only suitable source for disease research and therapy, study of human development, and the development of mouse models of the human immune system, termed “humanized mice.”
The practice and the promises predate Roe v. Wade. In over 100 years of fetal tissue research, not a single cure has been developed, and this more-or-less medieval research tool has produced only equivocal results even in basic biological studies.
Regulation of human fetal tissue research in the U.S. has a spotty record.
The executive order issued by President Bill Clinton, likewise on a Jan. 22 in 1993, was predicated on funding for transplantation studies, yet the only large studies funded by NIH produced “devastating” side effects in patients.
No clinical trials using fetal tissue have been supported since 2005. The Ethics Advisory Board, convened by the first Trump administration in 2020 to review proposals for fetal tissue research, rejected almost all proposals, primarily for ethical concerns. The report of the board shows that even supporters of fetal tissue research recognized serious ethical issues, with over one-third of votes unanimous or nearly unanimous for rejection of funding.
A further backlash against the use of tissues and cells from elective abortion was seen in the rejection of COVID-19 vaccines by a large swath of the American people for ethical reasons. As opposed to the despotic mandates of the Biden administration, simply acknowledging these concerns and creating vaccines using non-fetal cells, technologies which already exist, would have garnered public appreciation for the pharmaceutical industry, not to mention a larger share of the public getting vaccinated.
The new NIH policy represents a reblending of ethics and efficacy that will foster the best use of taxpayer dollars for avenues of research that have incredible promise.
The seminal comprehensive review of the history, science, and ethics of fetal tissue research was produced by members of the new Science Alliance for Life and Technology, who have labored for years alongside others to point out the failed science and ethics of human fetal tissue research. The review, as well as other work by SALT, documents modern, successful alternatives for research and clinical application, including adult and induced pluripotent stem cells, organoids, ethically obtained tissues, direct reprogramming, and gene-edited cells.
Here are just a few examples of breakthrough technologies that deserve investment:
Sickle cell anemia has been a scourge affecting about 100,000 U.S. patients, 20 million globally, causing severe pain, damaged organs, and shortened lifespan. But both cord blood stem cell transplants, as well as two new gene therapies recently approved by the Food and Drug Administration, have successfully treated sickle cell and released people from their suffering.
Using a technique called “direct reprogramming,” scientists have turned skin cells into retinal cells to restore sight to mice. While not yet ready for the clinic, this technique has great potential to treat conditions in which there is difficulty producing a therapeutic stem cell derivative.
A seventh patient has now been reported as “cured” of HIV after a specific adult stem cell transplant, and recent evidence suggests a wider pool of transplant donors can be used, as well as pathways to develop gene-edited cells for use in such transplants.
Human immune system (humanized) mice produced using aborted fetal tissue have both ethical and scientific shortcomings, which make them unsuitable for the development of human immunotherapies, human disease modeling, or human vaccine development. But two scientific groups have produced clinically relevant humanized mice. One group used cord blood stem cells and discarded postnatal surgical tissue to efficiently make humanized mice, while a second group used cord blood stem cells and hormonal conditioning to make the first mouse model with a complete functional human immune system.
Gene therapies are coming into their own, with an increasing number of treatments for genetic conditions under development. The story of the personalized gene therapy for Baby KJ is one of the most prominent and represents the vanguard of innovative, personalized genetic treatments.
An interview in The Wall Street Journal with the CEO of a company that is seeking to use genomic tools to obtain cures for a range of difficult diseases provides more detail about the potential for growth in the use of these ethical tools.
Companies are not only able to develop screening for rare genetic diseases and provide key early detection, but new ones are springing up to develop treatments for these diseases. Investment in better detection and innovative early treatments provide hope for individuals, families, and for the health of the nation, as well as a driving force for American innovation.
NIH’s new policy, which took effect immediately upon publication, is a triumph both for modernizing scientific research and for the taxpayer concerned about wasteful and ineffective government spending. It’s an announcement all Americans can celebrate.
We publish a variety of perspectives. Nothing written here is to be construed as representing the views of The Daily Signal.